The eleventh Citizens' Panel survey was carried out between November 2022 and February 2023.
The questions were on 3 different topics:
- The Tobacco Action Plan: to inform a refreshed plan to be published in Autumn 2023, which will support a tobacco-free Scotland
- Vaccination Motivations: to understand motivations behind continued uptake of COVID-19 vaccination
- Digital health and social care: to understand how people feel about the use of digital tools in health and social care
At the time of this survey, there were 1,015 Panel members from across all 32 local authority areas.
A total of 667 responses (66% response rate) were received, either by post, email or by telephone. This level of return provides data accurate to +/-3.79% at the overall Panel level. We do not break down the results into sub-categories (for example, sex or age) as they are not statistically significant. All comparisons that are made in this report are statistically significant, unless otherwise stated.
Key findings
The Tobacco Action Plan
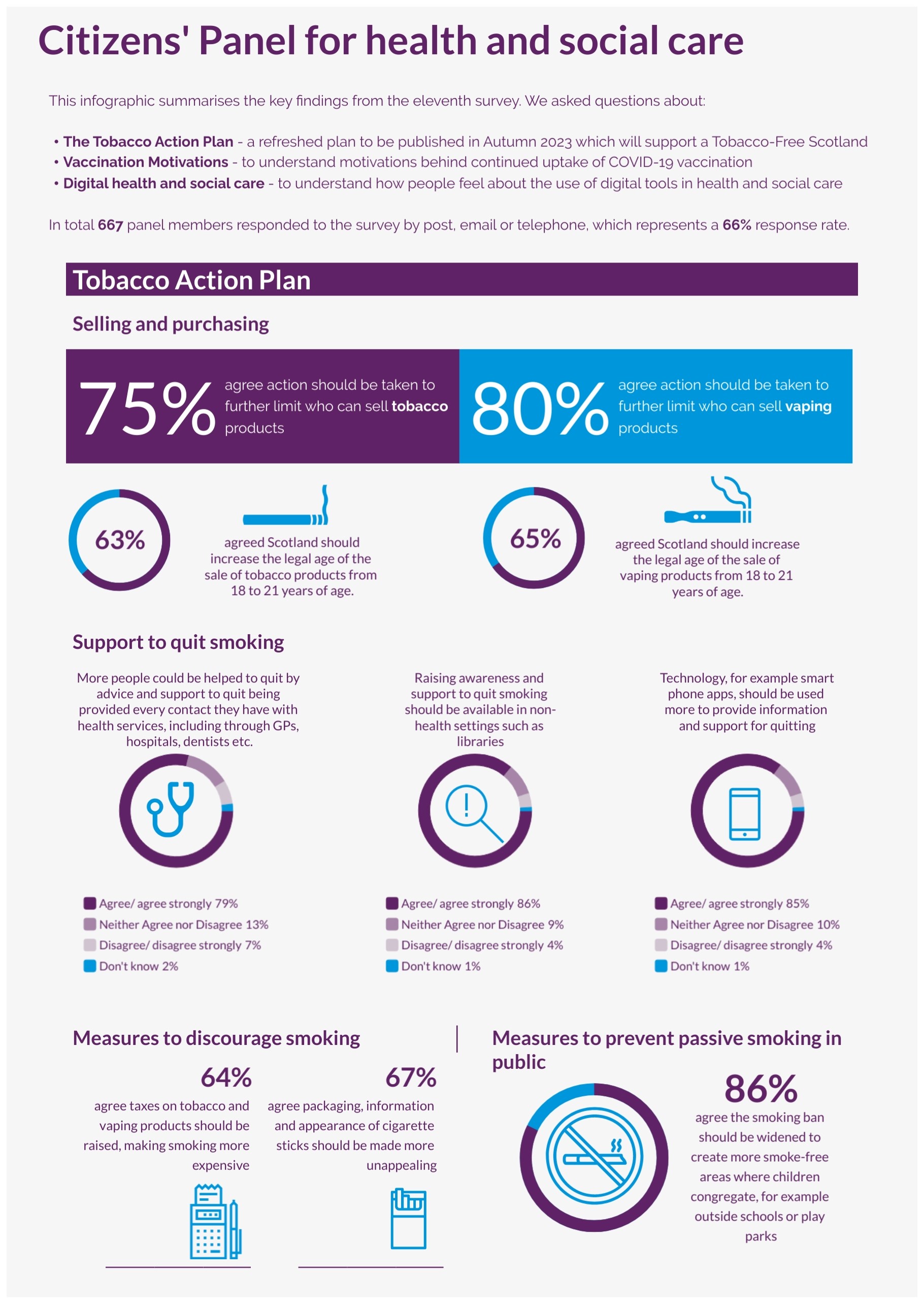
Selling and purchasing: Most respondents agreed that action should be taken to further limit who can sell nicotine vaping products (80%) and who can sell tobacco products (75%). Most respondents also agreed that Scotland should increase the legal age from 18 to 21 years for the sale of nicotine vaping products (65%) and tobacco products (63%), however nearly a quarter of respondents disagreed with these two options (23% and 25% respectively).
Support to quit smoking: Most agreed that raising awareness and support to quit smoking should be available in non-health settings such as libraries (86%) and that technology should be used more to provide information and support for quitting (85%). Most also agreed that more people could be helped to quit by advice and support being provided at every contact with health services (79%).
Measures to discourage smoking and prevent passive smoking: most agreed that packaging, information and appearance of cigarette sticks should be made more unappealing (67%). Most also agreed that taxes on tobacco and vaping products should be raised, making smoking more expensive (64%), though 23% disagreed with this. Almost 9 in 10 respondents (86%) agreed that the smoking ban should be widened to create more smoke-free areas where children congregate, for example, outside schools or play parks.
Recommendations
- Scottish Government should consider including all the measures that have the strongest public support in its Tobacco Action Plan 2023.
- Scottish Government should consider further consultation around more punitive measures, such as raising the age of purchase and raising taxation on tobacco and vaping products. After assessing the impact of these measures, these could also be implemented following a staged approach.
Vaccination motivations
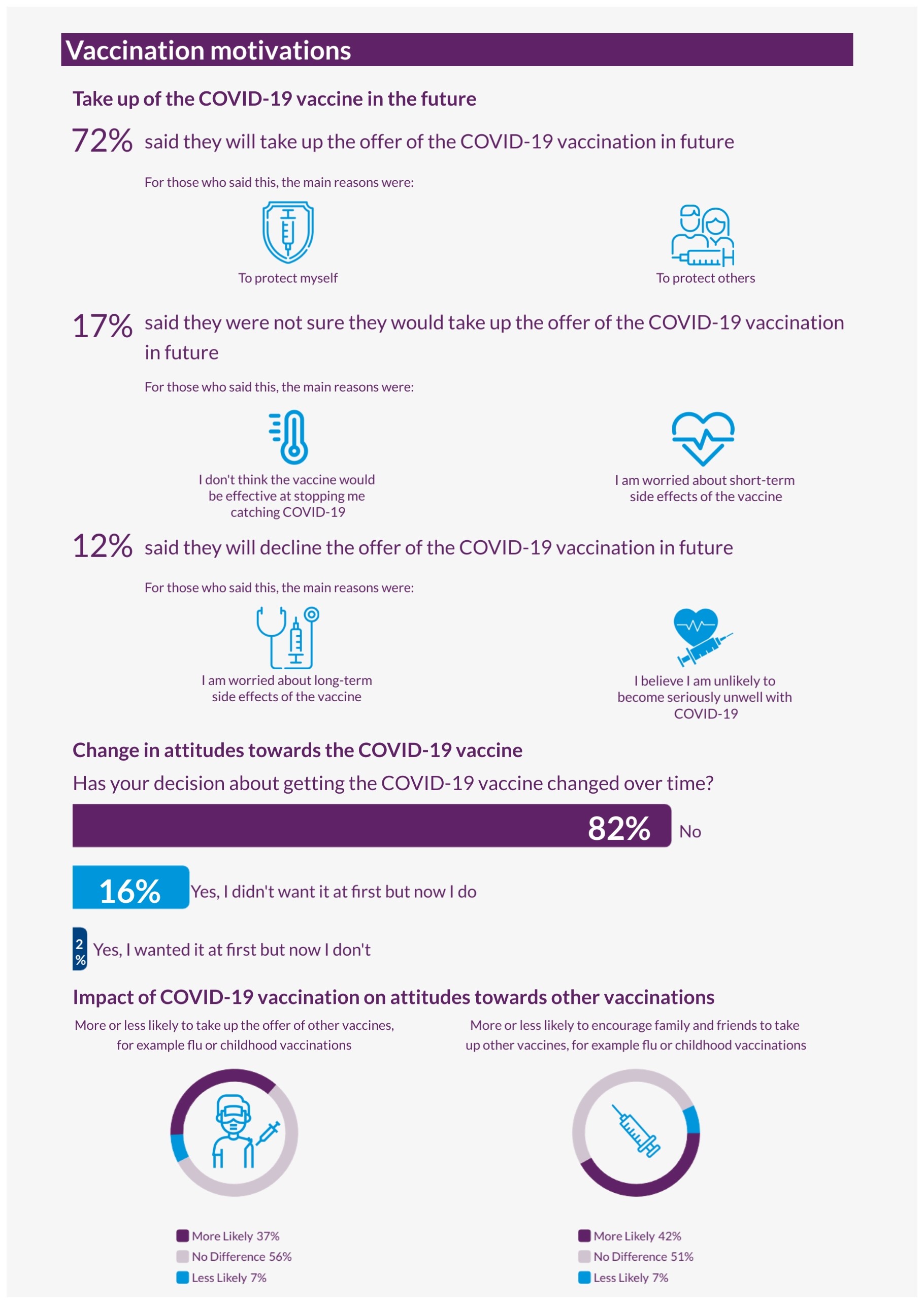
Take up of the COVID-19 vaccine in the future: Most respondents (72%) said that they would take up the offer of the COVID-19 vaccine in the future and their main reasons were to protect themselves (88%) and to protect others (82%). On the other hand, 12% said they would decline the offer in the future, mainly due to being worried about long-term side effects of the COVID-19 vaccine. 17% were not sure, either due to being worried about long-term side effects or not thinking that the vaccine would be effective in stopping them from catching COVID-19.
Change in attitudes towards the COVID-19 vaccine: Most respondents (82%) said that their decision about getting the COVID-19 vaccine has not changed over time, and this was mainly due to agreeing with the benefits of vaccinations or believing that it is important to get the vaccine to protect themselves and others. 16% said they wanted it at first but now they don’t and just 2% said that they didn’t want it at first but now they do. For those who changed their mind it was mainly due to being worried or having experienced side effects.
Impact of COVID-19 vaccination on attitudes towards other vaccinations:
- 42% said that their experience of the COVID-19 vaccine programme has made them more likely to encourage family and friends to take up the offer of other vaccines, for example, flu, baby or childhood vaccinations. On the other hand, 51% said it has made no difference in this, and 7% said it has made them less likely to do so.
- Just over one third of respondents (37%) said that their experience has made them more likely to take up the offer of other vaccines themselves, 56% said it has made no difference and 7% said it has made them less likely.
Recommendations
- Scottish Government and delivery partners to continue to consider vaccination experience and how to ensure positive and accessible vaccination experiences for all, as this is linked to broader attitudes towards vaccination. This necessitates working with a diverse range of key stakeholders, including NHS boards who deliver the vaccines, to drive improvements.
- Scottish Government and delivery partners to consider exploring people’s concerns further and their experiences around side effects. Developing further clear and accessible messaging around side effects, and the benefits and effectiveness of vaccination against serious illness may help address this. The work should consider aspects highlighted in this report, for example, linked to fertility or pregnancy, as well as potential equalities issues and barriers. This could be done in collaboration/partnership with groups who share these concerns, both those who are negative towards COVID-19 vaccination or unsure.
Digital health and social care
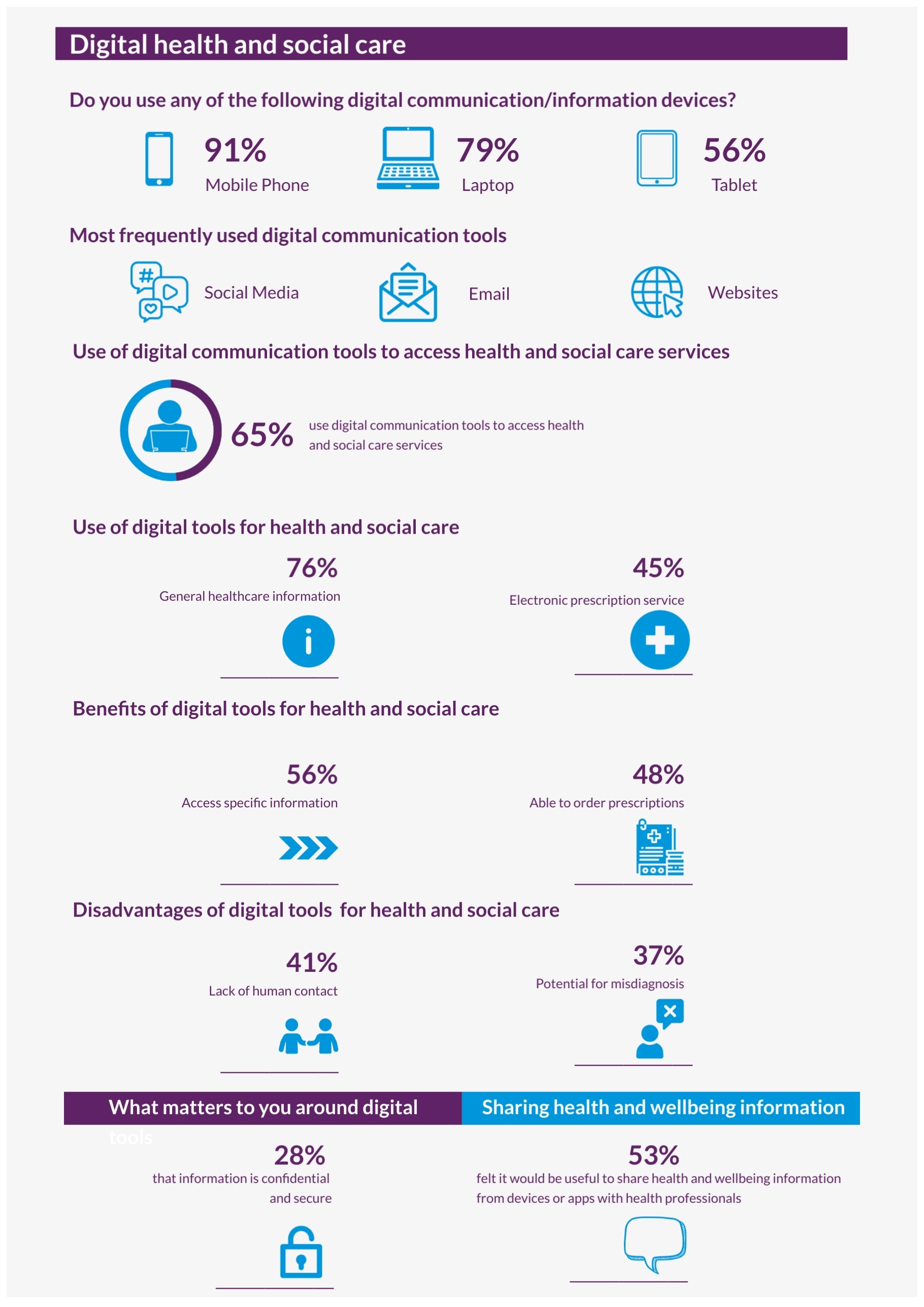
General use of digital tools: Most respondents used a mobile or smart phone (91%), a desktop or laptop computer (79%) or a tablet (56%). Just under 3 in 10 respondents used wearable technology such as a smart watch or Fitbit (29%). Only 3% of Panel members did not use any digital communication or information devices. A comparison to 2018 findings shows consistency in the percentage of respondents that use mobile phone or smart phones, and no significant change in the proportion of those who don’t use any digital devices. An increase in those using wearable technology was also found, and a decrease in the proportion using computers of tablets.
Panel members were most likely to use email (81%), websites (67%), social media (64%) or apps such as banking, shopping or health apps on a regular basis, at least once a day. However, a reasonably sized minority said that they never use social media (20%) or apps such as banking, shopping or health apps (12%).
Use of digital tools for health and social care: Just under two thirds of respondents (65%) said they used digital communication tools or technology to access health and social care services, for example, to access general health information or condition specific support, book appointments or get prescriptions. Of these respondents, 76% said they use digital tools to access general healthcare information and support services for example, NHS inform and 45% use an electronic prescription service.
For those who have used digital communication tools and technology to access health and social care support, the main benefits were being able to access information around specific health conditions or services (56%) and being able to order prescriptions (48%). In terms of the disadvantages or difficulties, 41% of respondents mentioned the lack of human contact (41%) and 37% spoke about the potential for misdiagnosis or information being misunderstood.
Benefits and disadvantages of using digital tools for care, and information-sharing: Respondents were asked what aspects of health and social care they believed would benefit from being online or more ‘digital’ and why. The top response was being able to book or change GP or other appointments (36%) and this was followed by access to video consultations (11%).
Over half of respondents (53%) felt it would be useful to share health and wellbeing information, for example, medical history and preferences, from their devices or apps with their health professionals or care providers. The main reasons for sharing health and wellbeing information from devices were where it would allow for improved or more information to be available (23%), would mean a faster process, service or diagnosis (12%) or would be easier, more accessible or convenient (9%). On the other hand, 21% of respondents had security or privacy concerns.
What mattered most to participants regarding the use of digital tools to access health and care was that information is confidential and kept secure (28%).
Recommendations
- Scottish Government and delivery partners to continue to use digital tools and technology to improve and provide access to services and support. Consider spreading this further and/or improving the digital-first approach to other services and aspects of care, for example, booking or changing appointments.
- Scottish Government and delivery partners to continue to engage with users around their preferences in using technology and digital tools in general, and specifically for health and care purposes, to monitor change in preferences and ways of using these tools.
- Scottish Government and delivery partners to ensure that equitable and appropriate non-digital routes are provided to all to access services and support, depending on individual needs, preferences and practicalities.
- Scottish Government and delivery partners to consider the public’s wish for assurance around security and privacy of information, regarding the use of digital tools and technology for health and care in general, and in the potential sharing of information between devices/apps and services more specifically. This would be in line with the Health and Social Care Data Strategy key principle around public trust and the ethical use of data for the public good. For this, they should consider:
- providing further public information and messaging around the benefits of the use of technology and information sharing
- providing clear, accessible and concise explanation of information governance processes in place
- aiming to increase public understanding, awareness and confidence in information security and privacy
Impact
Digital health and social care
Scottish Government note that the Citizens' Panel findings are consistent with Scottish Government engagement outputs and further research in the area.
Supporting the Scottish Government Renewal agenda, this work has informed the First Minister’s Renewal statement on the priorities of the Digital Front Door and supporting work, such as the integrated social care and health record that will deliver choice and flexibility, and empower people through online appointment booking, digital communication rather than physical letters, and the ability to deliver targeted public health information.
Scottish Government continue to draw upon these findings in discussions with policy colleagues and workstream leads to inform the development of digital options, particularly in regard to inclusion. Scottish Government remain committed to inclusion in developing of these services and throughout interaction with stakeholders, reiterating that Digital is a choice and non-digital options will remain available. Scottish Government are exploring this through a dedicated £2m Digital Inclusion Programme.
This work has supported Scottish Government in their focus on ensuring public trust and confidence in the use of digital technology, including the ethical use of data and, going forward, innovations such as Artificial Intelligence.
Scottish Government have drawn upon the Citizens' Panel findings for the annual update of the Health and Social Care Data Strategy, published in April 2024, and in the review of NHS inform (first phase June-October 2024), making recommendations to the Health and Social Care Management Board.
Scottish Government have used the Citizens' Panel findings as a useful reference when developing a suite of case studies highlighting the positive impacts of Digital in support of the Data Strategy. They have noted the Panel’s findings around public trust and the ethical use of data, and have focused on this aspect as a key part of their public engagement as they develop illustrative case studies and promote the publication of the Data Intelligence Network’s report into public attitudes and understanding of the use of health and social care data by public services.
Further information can be found at the links below:
- Programme for Government 2024-25: Serving Scotland (www.gov.scot) (see p35)
- Data Intelligence Network reports:
Tobacco Action Plan
The Tobacco and Vaping Framework, published in November 2023, and its implementation plan reflect action taken across the recommendations included in this work, including understanding based on these findings that vaping needs to be included within the plans. The introduction of the Tobacco and Vapes Bill has created a legislative vehicle for action in this area. If passed, it will raise the age of sale of tobacco products from 2027. It also provides the Scottish Minister with the powers to expand smoke-free spaces and create vape and heated tobacco-free spaces as well. Ash Scotland have led a review of the smoke-free hospital grounds legislation implementation and the potential for the expansion of smoke-free, vape-free or heated tobacco-free products. Scottish Government continue to implement the review of smoking cessation services through a public health action team at Public Heatlh Scotland, improving cessation services on the ground. Scottish Government have undertaken consultation on pack inserts for tobacco and continue to work together with the UK Government and other devolved administration on regulations that all administrations can consent to, with the aim of continuing to regulate packaging under a single UK-wide regime.
Further information can be found at the links below: