The fifteenth Citizens' Panel survey was carried out between November 2024 and February 2025.
The survey asked questions on three topics:
- Medicines Safety
- Long Term Conditions
- Preconception Health and Care
A total of 563 responses (57% response rate) were received either by post, email or telephone. This response rate provides data accurate to +/-4.13% at the overall Panel level. In this report we do not report results broken down into sub-categories (for example, sex or age) as they are not statistically significant. All findings and comparisons stated in this report are statistically significant, unless otherwise stated.
Public views on medicines safety
The first section of the questionnaire explored public views around medicines safety.
It was explained to Panel members that medicines are the most common intervention in healthcare, helping Scotland’s people live longer and healthier lives. However, medicines can cause harm to people, accounting for 1 in 10 hospital admissions worldwide. This harm also impacts the sustainability of services, and it's estimated that medication-related harm costs NHS Scotland up to £220 million each year.

- Thinking about over-the-counter or prescribed medication respondents are currently taking or have taken recently:
- 96% said they had a very good or good understanding of how to take the medication
- 92% said they had a very good or good understanding of the reason for taking the medication, and
- 73% said they had a very good or good understanding of the common side effects and risks related to the medication. 14% said they did not have much understanding, or had no understanding at all, of common side effects and risks related to the medication.
- Other than speaking to a healthcare professional, respondents were most likely to find information about a medicine by reading the information leaflet included in medication packaging (85%), visiting an NHS Scotland website (71%) or using an online search engine (61%). Some would ask others, such as family and friends (13%).
- If looking for more information about medicines online, the majority of respondents (88%) said that NHS branding, such as the NHS logo, would help them feel confident that the information is reliable and up-to-date. More than 6 in 10 said a recommendation from a healthcare professional to use the online source would give them this confidence (62%).
- Over half of the respondents said they had experienced side effects or unintended effects from a medicine (57%), 37% had not experienced any and 6% were unsure. This question relied on individuals’ understanding of what may be a side effect, which could differ from a clinician’s perspective. The question did not specify severity or whether these may have been known or expected side effects, for example, listed in the medicine leaflet.
- From those who had experienced side effects, most had spoken to a doctor, nurse or pharmacist about the side effects they experienced (84%, n= 313). 11% (n=313) had not talked about their side effects to anyone, mostly because they thought their side effects were minor or common (60%, n=33).
- The majority of respondents either agreed or strongly agreed with the statements provided:
- 99% agreed it is important to understand the purpose, benefits and risks of any medications they are taking.
- 98% agreed they would expect NHS Scotland to gather and analyse data on medicines-related harm to improve safety.
- 95% agreed that if they realise they are experiencing side effects from a medication they take, they would be willing to tell a healthcare professional.
- 93% agreed that they are willing to be involved in discussions about medication they take, including risks and potential harms.
- 83% agreed they have the help and support they need to understand the medicines they take. 10% were neutral and 8% disagreed that they have the support they need.
- When asked what matters most about the safe use of medicines, around 3 in 10 respondents (30%) discussed side effects. They mentioned ensuring clear communication on the risks of side effects and what to do if they experience them. 20% said they wanted to know that any medication they are taking is necessary and will be effective in treating their health condition. 19% said they would want to know that medicines are safe and have been rigorously tested. 18% wanted to know that information provided on medicines such as in the packaging is clear, accessible and accurate. Further aspects mentioned were: having clear instructions on how to take medication (11%); having confidence in the prescriber, being able to ask questions and have clear explanations (10%); knowing that benefits outweigh side effects (9%); and that the medicines are NHS approved (1%). 6% touched on multimorbidity and polypharmacy. They said that what matters most is knowing how medication will react with other medication and conditions.
Recommendations
Based on these findings Healthcare Improvement Scotland makes the following recommendations to Scottish Government and relevant stakeholders. Recommendations are outlined in further detail in the full report.
- Consider development of resources that support the public to understand the information, resources and processes that help people to take medicines safely and effectively. This should build upon the public’s trust and willingness, seeking opportunities to engage with the public and patient representative groups in co-creating resources. This should also include work to encourage more widespread awareness and use of resources. It would be worthwhile considering how NHS branding is used in this area and whether its use could be further expanded where appropriate to support public confidence. Also consider how to obtain support from existing local arrangements and other partners, for example Community Pharmacy Scotland.
- Ensure that information around medicines is available to the public in a range of formats, for example, in physical leaflets and online resources, and that it is provided to patients according to their preferences and accessibility needs, including through one-to-one discussion with healthcare staff. Ensure there are suitable avenues to ask questions and support understanding of medicines information. This could be for example about how medication may react with other medication or herbal remedies. Also consider how to address information needs where non-standard processes are in place. This could be where medicines are knowingly used outwith their product licence, for instance in treating some types of cancer, or in self-medication. In these cases, patients may not have all the information available to hand in the patient information leaflet.
- Based on the prevalence of the public’s use of digital tools to find medicines-related information, consider further work to explore in-depth how the public use Artificial Intelligence (AI) tools to find and understand healthcare information, and particularly information relating to medicines, aiming to help understand how to address potential risks of misinformation. Also consider the role of signposting from healthcare professionals to address risk posed by AI information sources.
- Consider actions to support increased public understanding of why medicines are beneficial and necessary, as well as around side effects and risks related to medicines. This should build upon public trust in the NHS and healthcare staff. For example, this could be through using the BRAN questions and a realistic medicine approach, and increased signposting to relevant resources and information.
- Take action to promote and support public awareness of the Yellow Card Scheme to improve under-reporting of medicines’ side effects. Combined with this, improve how NHS Scotland draws learning from the data that are collected and analysed through the Yellow Card Scheme, and other data collected locally such as through Datix; and then uses this learning to identify and take specific actions to improve medicines safety across Scotland.
- Consider work to further understand and identify where challenges relating to medicines safety may have more significant impact. This would include exploring potential barriers and enablers for particular groups. This could be for example around understanding side effects and risks, engaging in discussing medicines, and ensuring people have enough support to understand the medications they take.
Public views on long term conditions
The second section of the questionnaire explored public views around long term conditions.
It was explained to panel members that over a third of the people across Scotland have a long term condition. A long term condition is a physical or mental health condition that lasts a year or longer, which impacts on a person’s daily life and may require ongoing care and support. This includes conditions such as asthma, diabetes, heart disease and bipolar disorder. Long term conditions are important because as people live longer, the number of people with long term conditions is also growing, putting additional pressure on the NHS.
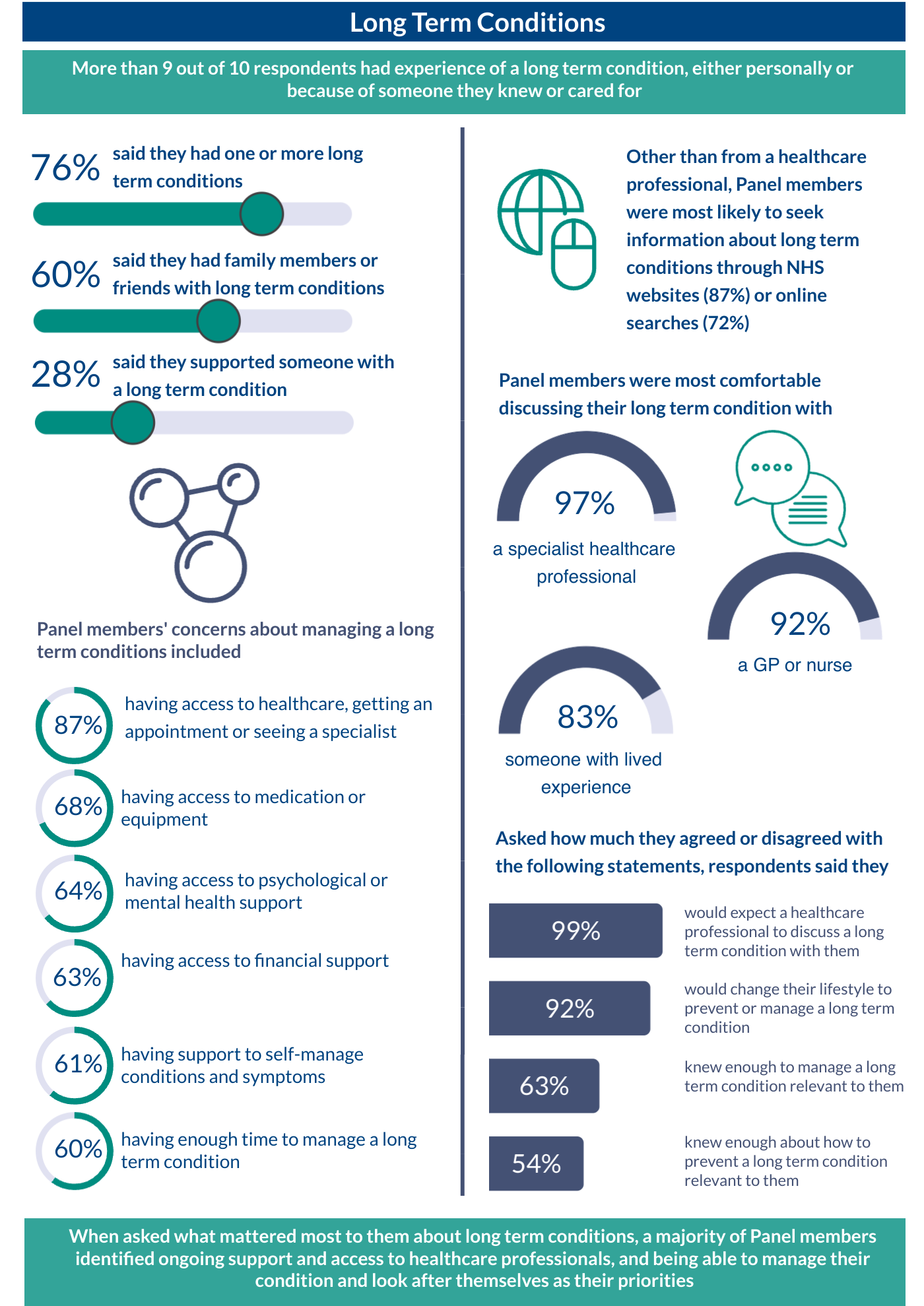
- Over 3 in 4 respondents (76%) said they personally have one or more long term conditions. Nearly 2 out of 3 (60%) said they have family members or friends with long term conditions. Just under 1 out of 3 (28%) said they provide care or support for someone with a long term condition. Less than 1 in 10 respondents (8%) answered none of the above to this question. It should be noted that the proportion of respondents who had a long term condition is higher for the survey than the data we hold on Panel members.
- Other than talking to a healthcare professional, Panel members were most likely to look for information about long term conditions on an NHS website, such as NHS Inform or local health board webpages (87%). They were also likely to do an online search (72%) or approach a third sector organisation or group (55%).
- Respondents were asked how comfortable they would feel discussing long term conditions with various people, including healthcare professionals. It was explained to Panel members that this could be for themselves now or in the future, a family member or someone they care for. Respondents were most likely to feel comfortable with a specialist healthcare professional (97%), primary care professional such as a GP or nurse (92%), someone with lived experience of the condition (83%) or pharmacist (80%). Panel members were most likely to say they would not be very comfortable or not at all comfortable discussing a long term condition with someone that practices alternative therapies (35%) or someone who knows the patient such as a coach or teacher (28%).
- The biggest concerns for Panel members about managing long term conditions included:
- access to healthcare, for example getting an appointment or being able to see a specialist (87%)
- access to medication and/or equipment (68%)
- psychological and mental health support (64%)
- financial support (63%), and
- support to self-manage conditions and symptoms (61%).
- Panel members were asked to state how much they agreed or disagreed with various statements about long term conditions. Most Panel members agreed with all statements:
- 99% agreed if they were to have a long term condition, they would expect a healthcare professional to discuss with them how it might impact their life.
- 92% agreed if they were advised to change something in their lifestyle to prevent or manage a long term condition, they would be motivated to do this.
- 63% agreed they felt they knew enough about how to manage long term conditions that were relevant to them.
- 54% agreed they knew enough about how to prevent long term conditions that were relevant to them.
- When asked what matters most about long term conditions, 26% spoke about ensuring a broad range of support being available. 19% mentioned having ongoing access to healthcare professionals and 17% spoke about being able to manage the condition or look after themselves. 16% mentioned the impact of their condition on quality of life and on family members, and 11% identified getting the right care or treatment.
Recommendations
Based on these findings Healthcare Improvement Scotland makes the following recommendations to the Scottish Government and relevant stakeholders. Recommendations are outlined in further detail in the full report.
- Consider that policy relating to long term conditions explicitly acknowledges that these impact on a great number of people, directly (as patients and carers) and indirectly (as members of the wider support networks). This should include acknowledgement of the very broad range of individual experiences shaped not just by the specific condition affecting the patient, but also by the individual's personal circumstances and their perceived support needs. In addition, these findings recognise that there is a range of overarching concerns which may be relevant to large numbers of people who are affected by different long term conditions. This supports the argument for an overarching framework for long term conditions addressing issues of common interest as a way forward.
- Consider how long term conditions are approached across health and care, ensuring targeted support for healthcare professionals and the public. This might include:
- offering appropriate training to healthcare professionals to support meaningful person-centred conversations with patients and carers. This would address their need for a holistic perspective (including medical and non-medical elements of their experience) and enhancing their understanding and ability to prevent and navigate conditions
- considering how medical and non-medical support offers can be integrated with a focus on individual need, patient preferences and potential to self-manage their condition, and
- reflecting on how to ensure inclusiveness across the framework so that individuals with specific needs have access to care in a way that is appropriate to their requirements.
- Consider further work to explore how the public use AI-supported search engines and tools to find and understand healthcare information related to long term conditions and address potential risks of misinformation resulting from this. It could further include strengthening the NHS online brand as a guarantor for accessible, reliable and evidence-based information. Also consider information signposting by healthcare professionals to counter risks from AI-generated information sources.
- Consider strengthening the case for patient and public engagement around long term conditions to support mutual learning. This should include the co-design and co-creation of local support networks incorporating and reaching beyond medical care.
Public views on preconception health and care
The third section of the questionnaire explored public views around preconception health and care.
Preconception health relates to the health and wellbeing of people during their childbearing years. It is shaped by the health behaviours and environment of both women and men. Preconception health is an important topic because it can influence fertility, early child development, and can prevent harm to future generations. We recognise that the area of preconception health is closely related to fields such as reproductive health and population health, hence these findings may be relevant to inform thinking in further fields.
Panel members were told that their views on this topic were important even if they are not currently considering pregnancy or having children. To answer the survey questions, members were asked to think about themselves currently, or in the past or future, and they could also think about a partner or family member.
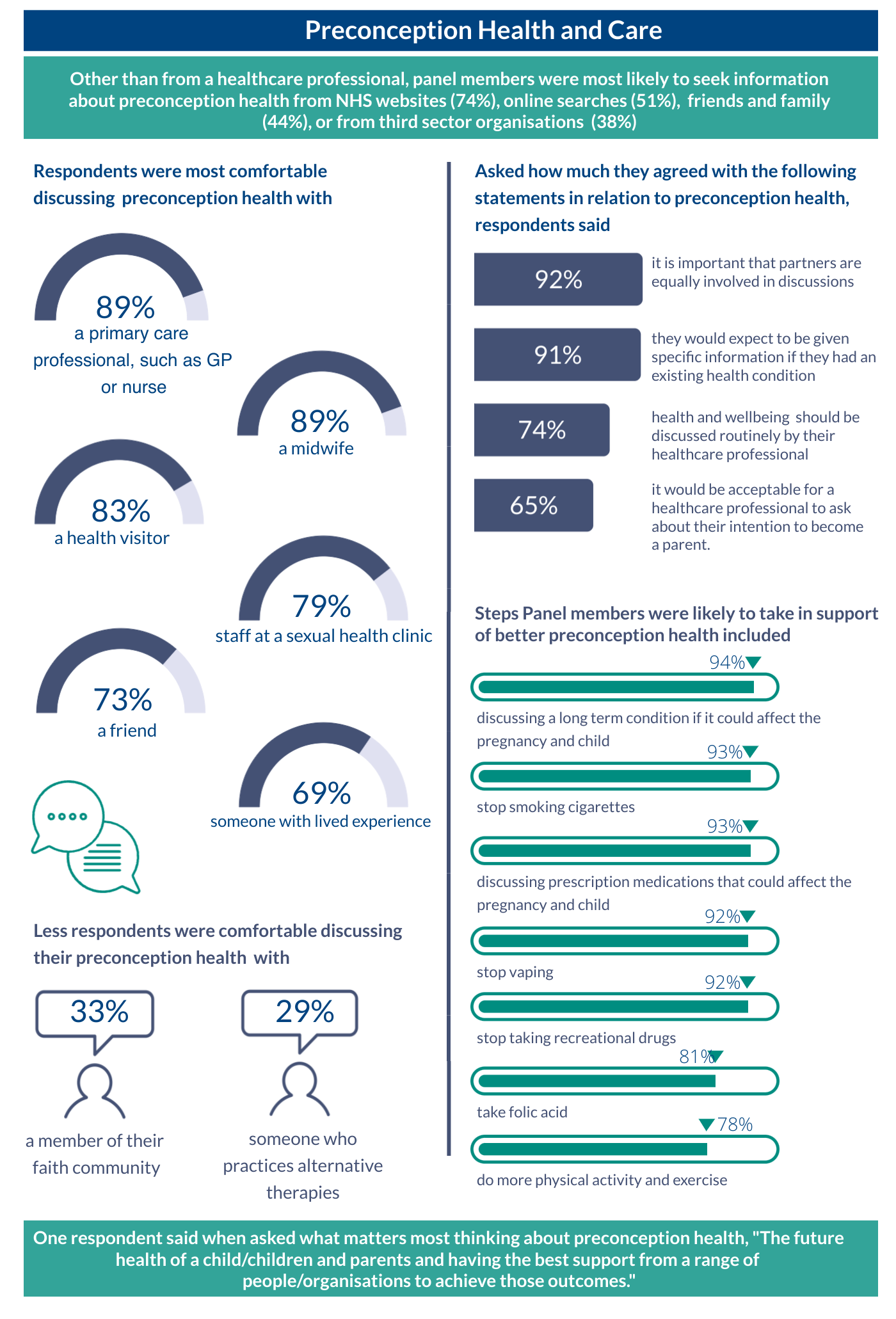
- Other than a health care professional, to find out more information about preconception health respondents were most likely to turn to an NHS website (74%), or an online search engine (51%). They were also likely to speak to friends and family (44%) or a charity (38%). 2% said they would only speak to a healthcare professional.
- When asked whether they would be comfortable discussing preconception health with different people and roles, respondents selected all suggested options. However, all options also had some not being comfortable with them. Most were comfortable discussing preconception health with healthcare professionals such as in primary care (89%), a midwife (89%), or health visitor (83%). Further avenues that were comfortable to most included discussing preconception health with a friend (73%) or someone with lived experience (69%).
- Most agreed that it is important that partners are equally involved in conversations about preconception health (92%). Most also agreed that they would expect to be given specific information by a healthcare professional about preconception health if they had a pre-existing health condition (91%). Most thought that preconception health should be discussed routinely between people of childbearing age and healthcare professionals (74%). Over half said they would find it acceptable for a healthcare professional, such as a GP or nurse, to ask them about their intention to become a parent (65%). It is important to note, however, that more than 1 in 10 (13%) said they would not find it acceptable for a healthcare professional to ask them about their intention to become a parent.
- When asked if they would be willing to try a range of things to improve preconception health if they were to consider having a child, most respondents said they would be willing to try all actions included in this survey. For example, this could be discussing their long term condition(s) that could affect the pregnancy and child (94%), or to stop smoking cigarettes (93%). On the other hand, all actions had a small number of respondents saying that they would not be willing to do them.
- Respondents were asked about what matters most to them when thinking about preconception health. Over 4 in 10 respondents mentioned parents having good health (42%), and others mentioned access to information and advice (23%), and ensuring the baby’s health and safety (15%).
Recommendations
Based on these findings Healthcare Improvement Scotland makes the following recommendations to the Scottish Government and relevant stakeholders. Recommendations are outlined in further detail in the full report.
- Ensure that policy relating to preconception health acknowledges that preconception health is perceived as beyond being a “medical” issue, and as intersecting with a range of aspects in people’s lives and identities. Policy content should address and acknowledge this accordingly.
- Consider how to increase awareness about the relevance and importance of preconception health at a population level. Include addressing sensitivities around preconception discussions, and the stigma attached to choosing not to have a child. This would also include increasing understanding of the benefits and risks of behaviours.
- Consider how preconception health is approached across health and care, ensuring support for both healthcare professionals and the public. This could include training for healthcare professionals, considering how individuals can discuss preconception health routinely and the potential role of primary care professionals, community pharmacies, and midwives relating to preconception health. There should also be a way for individuals to opt-out from discussing preconception health. Also consider how to involve partners equally in preconception health discussions.
- Consider development of further resources that support the public in understanding and engaging around preconception health. This should build upon the public’s interest and willingness to discuss, and adopt a culturally sensitive and person-centred approach, based on real-world needs.
- Ensure that information around preconception health is available to the public in a range of formats, to enable discussions in different contexts and according to their preferences and accessibility needs, including through one-to-one discussion with healthcare staff.
- Consider work to gain a further in-depth understanding of preconception aspects highlighted in these findings. This should include exploring information needs, the use of AI tools to find information, how to equally involve partners, barriers and enablers for particular groups, including regarding behaviour change.
Impact
Scottish Government have noted the significant impact and input from this Citizens' Panel work.
Long term conditions
These findings have been used by Scottish Government in developing the Long Term Conditions Framework and relevant outcomes for improvement. Scottish Government highlight the importance of this work in eliciting rich insights from a wide range of participants and demonstrating what matters most to people with long term conditions. The Framework is due to be published by Scottish Government in December 2025, with the first in a series of action plans in March 2026.
Preconception health
This work has supported Scottish Government across a range of teams, including the Preconception Collaborative. They highlight the importance of this work, as this is the first time Scottish Government have heard directly from members of the public on this topic, identifying key areas that require renewed focus. This work is being used to address a commitment in Programme for Government: Embedding early conversations on preparing for pregnancy into routine health care, to optimise preconception health and care. The findings are being used within a cohesive preconception delivery framework model, aiming to identify drivers for shifts in culture and actions to optimise preconception health and care. Scottish Government are using this work to develop more targeted and effective messaging, ensuring inclusive communication that is responsive to the needs and concerns of diverse communities.