The ninth Citizens' Panel survey was carried out in between January and April 2022. We asked questions about Public Engagement in health and social care service design and change, COVID-19 vaccination programme inclusion and COVID Status Certification.
At the time of this survey in early 2022, there were 949 Panel members from across all 32 local authority areas.
A total of 507 responses (53% response rate) were received, either by post, email or by telephone. This level of return provides data accurate to +/-4.8% at the overall Panel level. In this report we do not report results broken down into sub-categories, for example, gender or age, as they are not statistically significant. All comparisons made in this report are statistically significant, unless otherwise stated.
Key findings
Public Engagement in health and social care service design and change
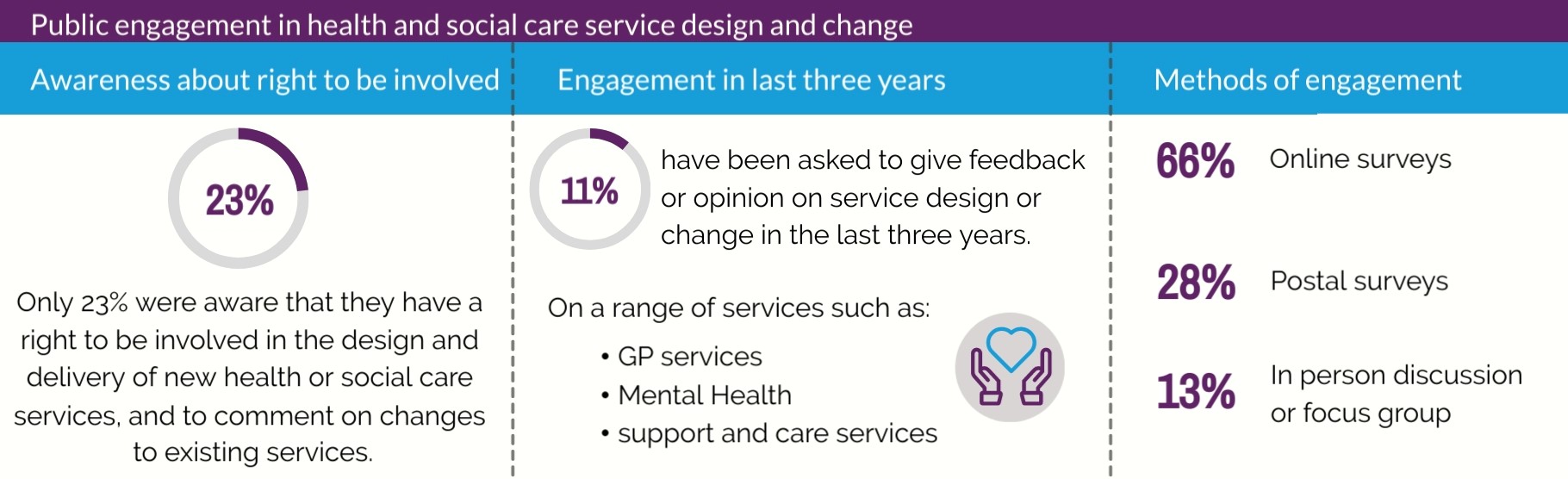
Just under one quarter of respondents said that ‘yes’ they were aware that people across Scotland have the right to get involved in the design and delivery of new health or social care services, and to comment on changes to existing services, beyond giving feedback through the Citizens’ Panel.
Over the last three years, 11% of respondents have been asked to give feedback or opinion on service design or change in local health or social care. The service that respondents were asked to provide feedback or opinion on varied from GP services to mental health and support and care. The most common form of engagement was by taking part in an online survey (66%).
All who had been involved in engagement were asked how they would rate their experience in this engagement. Overall, 45% said that their experience was either very positive or positive, 34% said it was neither positive nor negative and 19% said that their experience was negative. The most common reasons for having a positive experience were the fact that they got a chance to give their views/ felt they could make a difference (38%) or that the consultation or engagement process went well/ was easy to respond to/ take part in (25%). Where respondents were neutral or not as positive about their experience, the most common response was that they haven’t seen any changes as a result or don’t know the impact of their input (20%).
The aspects that matter most to respondents about being involved in the design of new health or social care services or changing existing services were: being able to improve local services (65%), knowing that feedback could lead to changes and inform decision making (56%) and having a say on health and social care issues that matter to them (45%).
Recommendations
We make the following recommendations to the Scottish Government, NHS boards, Health and Social Care Partnerships and Local Authorities:
- Incorporate the findings of the above survey into the review of ‘Planning with People – Community Engagement and participation guidance for health and social care’ (published March 2021 by Scottish Government and COSLA).
- Continue to develop existing strategies for public engagement to encourage all communities to participate in health and social care service design, including:
- raising awareness of the public’s right to get involved in the design and delivery of new health and social care services
- informing the public about proposed changes to health and social care services throughout an engagement process, and
- providing feedback on the results and/or impact of the engagement to those who took part.
- Healthcare Improvement Scotland – Community Engagement to work collaboratively with partners to develop training opportunities for staff to increase confidence when involving people.
COVID-19 vaccination programme inclusion
94% of respondents said that they have received at least one vaccination, with 85% having received their first, second and booster/ third vaccinations, which was the maximum available at that point in time. Just 4% of respondents had not received any COVID-19 vaccinations.
The most common method of being informed about their COVID-19 vaccine was by being notified about the appointment through a blue letter in the post. This was the case for all three vaccines, with 57% of respondents noting this was how they were informed about their first vaccine, 54% for the second vaccine and 40% for the third vaccine.
Where respondents had used either the online booking system or the National Vaccination Helpline to either book or change their vaccine appointment, they were asked how easy or difficult they found using these. The experience of using the online booking system was largely positive, with 85% stating they found this either very easy or somewhat easy to use. A total of 57% of the respondents who had used the National Vaccination Helpline said they found this very or somewhat easy to use.
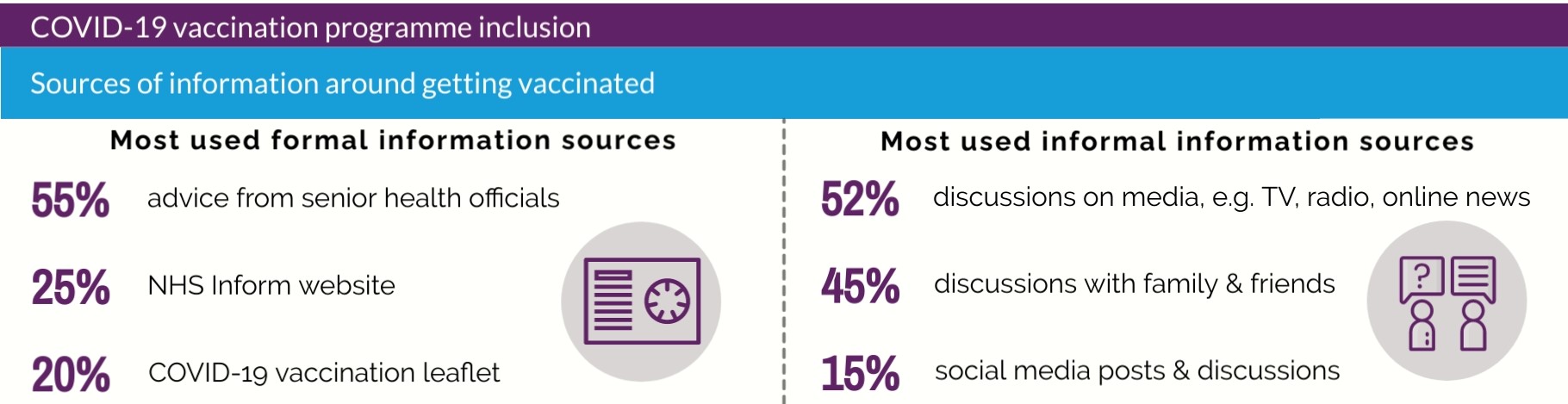
When respondents were asked what sources of information they used to help decide whether to get the COVID-19 vaccine or not, the most used sources were: advice from senior health officials (55%), discussions in the media (TV, radio, online news websites) (52%) and discussions with family and friends (45%). With respect to formal NHS information sources, 25% had used the NHS Inform website and 20% a COVID-19 vaccination leaflet.
Overall, 89% of respondents stated that they think the COVID-19 vaccination programme in Scotland was either very accessible or somewhat accessible, compared to just 3% who stated that they believed it to be either somewhat inaccessible or not accessible at all.
Those who had been vaccinated were asked how accessible they found different aspects of their COVID-19 vaccination process. Most respondents found all aspects around COVID-19 vaccination accessible. Aspects that were most likely to be accessible were vaccination venue accessibility features (such as wheelchair access, quiet rooms etc.) (94%), information on the vaccination (93%), location of the vaccination venue (91%) and getting to the vaccination appointment (91%).
A small percentage of respondents noted aspects of COVID-19 vaccination as somewhat inaccessible or not accessible at all: 5% found the process of vaccination itself, for example queuing and length of wait, somewhat inaccessible and 2% said it was not accessible at all. 4% found travel to the vaccination venue to be somewhat inaccessible, and 3% found it not accessible at all.
Respondents were then asked, in their experience, if there was anything that would make their COVID-19 vaccinations easier and more accessible for them. The most common response was that nothing could have been done to make their COVID-19 vaccination easier and more accessible for them (39%). Where suggestions for improvement were made, they were around providing vaccinations at more local centres/ at GP practices (19%), improved organisation at the venue, for example signage, seating, checking in (11%) and an improved online booking system (6%).
Participants were also asked their views on equalities data collection at their COVID-19 vaccination appointment, specifically around the collection of ethnicity information. Information around ethnicity is currently being collected through the vaccination programme to help the NHS, Scottish Government and partners to understand health inequalities, and through the survey we sought insight into how the public feel about this.
When asked if they would be comfortable to be asked about their ethnicity at their COVID-19 vaccination appointment or on the online booking portal, 79% said ‘yes’ they would be comfortable if asked about their ethnicity. 11% said ‘no’ and 10% said ‘I’m not sure’, with some saying that ethnicity is not relevant to COVID-19 vaccination or healthcare in general
Recommendations
We make the following recommendations for the Scottish Government and delivery partners for future vaccination programmes:
- Continue to provide clear and valued public information, offer diverse and flexible delivery processes and work with the third sector to facilitate vaccination uptake.
- Ensure that people are offered appointments at the most convenient site for their vaccine. Maintaining the person-centred approach in the COVID-19 vaccination programme, people should continue to be able to reschedule appointments and choose different venues to receive the vaccine. People should also be offered the flexibility to have their vaccine in a different NHS board area. This should also be considered in the context of wider vaccination programmes, not just COVID-19.
- Ensure that vaccination clinics are fully accessible to all and suit the needs of the individuals attending. Ensure that support needs are met in line with recorded requirements, for example providing a quiet room, short queue for those who can’t stand, wheelchair access, an interpreter or sight guide, or accompaniment by a carer.
- Provide accessible localised information on how to get to vaccination locations, liaising with local authorities, services and third sector organisations. This should also include details on free and subsidised travel. Ensure that specialised services are provided where there is no provision of public transport.
- Involve local communities and third sector partners in decisions about venue use, auditing accessibility of venues and supporting people to attend.
- Ensure there is a simple, well publicised and accessible route for individuals to request support if they have specific requirements to access all aspects of vaccination, including information.
- Continue to seek and respond to feedback of service users using the National Vaccination Helpline.
- Continue to utilise the significant influence of advice from senior health officials in further major health interventions, as well as continuing to develop information to be shared more informally, becoming part of informal conversations with family and friends.
- Continue collecting ethnicity data at point of vaccination, and communicate further the purpose and benefits to support the public’s understanding.
- Ensure learning around accessibility from the COVID-19 vaccination programme is collected, consolidated and shared with all relevant bodies and organisations, as well as with the public, in order to shape future policy around vaccination and major health interventions.
COVID Status Certification

When asked the extent to which they agreed or disagreed with several statements about COVID Status Certification, respondents were most likely to state that they agreed that:
- COVID Status Certification makes places, spaces and events safer to visit (70% strongly agree or agree).
- I trust how the COVID Status Certification scheme uses my data and information (50% strongly agree or agree).
Respondents were more likely to either disagree or strongly disagree with the following statements:
- I am concerned about using COVID Status Certification (56% disagree or strongly disagree).
- Certification unfairly prevents people from doing things they want to do (56% disagree or strongly disagree).
Most respondents (79%) said COVID Status Certification has not had any influence on their decision to get vaccinated.
Over three quarters of respondents (78%) said the ability to use a negative test result (Lateral Flow Test (LFT) or PCR) instead of proof of COVID-19 vaccination did not make a difference in terms of their likely use of COVID Status Certification. 7% said they would be more likely to use COVID Status Certification after introducing the possibility of testing whereas 9% said they would be less likely.
When asked about the ease of obtaining and using COVID Status Certification, 33% of respondents said they had not used it. Of those who had used COVID Status Certification, 68% said they found this either very easy or somewhat easy to use, 19% said it was neither easy nor difficult and 14% said they found it difficult to use.
When asked what would make them decide not to use COVID Status Certification, the most common response was that ‘nothing’ would make them not use COVID Status Certification (54%). 9% expressed concerns over data security, 8% said that they do not go to the sort of places where it was required, 7% do not support Certification and 7% said they have not needed to use Certification. However, as 33% had not used COVID Status Certification, as mentioned above, these concerns may be perceptions rather than based on their experience.
When asked what would make them not visit venues that required COVID Status Certification, again, the most common response was that nothing would make respondents not visit venues where they would be asked for COVID Status Certification (49%).
When asked about potential concerns around COVID Status Certification excluding people, just over one quarter of respondents (27%) said that they did not have any concerns. The most common concern was about people not being able to access the necessary technology, for example internet, computer or smartphone (20%). This was followed by unvaccinated people being excluded (10%). It is worth noting that many of these comments were made with specific reference to those who are medically exempt and cannot be vaccinated. It is important to note that these are public perceptions and not necessarily based on people’s experiences or the policies and practices in place. For example, while non-digital and alternative routes to obtain COVID Status Certification were available, 20% of the respondents continued to have concerns around potential exclusion around digital access or unvaccinated people. These findings may suggest that the Panel members do not feel that the mitigations put in place were enough to resolve their concerns, or they may have not been aware of the steps taken to minimise potential exclusion, requiring more extensive communication around these options.
Recommendations
We make the following recommendations to Scottish Government, in the eventuality that COVID Status Certification was under consideration to be reintroduced or a similar scheme developed:
- Continue to use a digital-first approach, as digital tools are mostly well received and seen as easy to use. However, continue to provide equal access via non-digital routes and support to users when they face challenges with technology.
- Ensure the public has up-to-date and accessible information about COVID Status Certification, including:
- the importance and need for COVID Status Certification, to increase understanding for those that may not support certification in general, if certification was under consideration to be reintroduced or a similar scheme to be developed
- the different routes to COVID Status Certification and how those eligible can access exemptions
- the scope of COVID Status Certification and its distinction from non-domestic certification to reinforce understanding, as there was some remaining confusion around domestic COVID Status Certification versus COVID Status Certification for international travel, and
- the use of personal data and data protection.
- Ensure strong engagement with those most likely to be affected by COVID Status Certification, prior to activating it, as highlighted in ‘Planning with People – Community Engagement and participation guidance for health and social care’.
- Continue to explore the public’s experiences and views around COVID Status Certification in terms of the positive impacts and the range of challenges and potential barriers to access highlighted in this report.
- Consider the impact and efficacy of COVID Status Certification to inform future planning and policy decisions, for example whether there may be influence on vaccine uptake.
- Ensure learning from COVID Status Certification is collected, consolidated and shared with all relevant bodies and organisations, as well as with the public, in order to shape future policy and major health interventions.
Impact
Scottish Government topic sponsors fedback the short term impacts from the Citizens' Panel 9 survey results which will influence healthcare policy and services.
COVID Status Certification
The report provided valuable insight into experiences of domestic, mandatory Covid Status Certification, with findings supporting an assessment on the efficacy and impact of the policy. The technical guides for protective measures include the evidence from the results, which will form part of the evidence base should certification need reintroduced.
Public Engagement
The public engagement questions informed the 2023 review of ‘Planning with People'. This is community engagement and participation guidance for health and social care. Planning with People describes the importance of good meaningful engagement (updated 2024).
Inclusive Vaccination
Following the publication of Citizen’s Panel 9, the Scottish Vaccination and Immunisation Programme (SVIP) has since transferred overall responsibility for vaccinations in Scotland to Public Health Scotland (PHS), with territorial NHS boards continuing to have responsibility for local delivery.
The COVID-19 programme is transitioning from a pandemic response to that of routine immunisation and has been significantly scaled back, with only those members of the public at higher risk being offered vaccination at fewer venues, during seasonal campaigns. As COVID-19 settles into a seasonal pattern, NHS boards along with support from PHS will use the lessons learned from the COVID-19 programme to embed a long term strategy for making vaccination venues as accessible and fit for purpose as possible.
The public are still able to source a flu and COVID-19 clinic anywhere in Scotland by using the national vaccination helpline and online booking portal. As part of SVIP, Scottish Government are considering a new end-to-end digital system for booking and recording all vaccines.
The introduction of recording of ethnicity data through the COVID-19 programme has significantly enhanced the understanding of inequalities in vaccine uptake. Guided by the principles from Citizen’s Panel 9, the Scottish Government, PHS and NHS boards are collaborating to ensure inclusivity in all vaccination programmes, with particular focus on using vaccinations to tackle inequalities. PHS and NHS boards continue to collect and analyse ethnicity data and digital work is ongoing to understand the factors contributing to poor health outcomes. This will help target groups with low vaccine uptake more effectively.
As part of the SVIP there will be a dedicated workstream for inclusion and equity and PHS will build upon their third sector networks to engage key organisations and stakeholders in shaping how programmes are delivered.