The seventh Citizens' Panel survey was carried out in November and December 2020. We asked questions about health and social care experience during the COVID-19 pandemic and priorities for health and social care in the future.
The survey ran from 2 November 2020 until 4 January 2021, just as COVID-19 case numbers were increasing and social restrictions were tightening again. A total of 652 responses (56% response rate) were received, either by post, email or by telephone.
Conclusions
- A considerably larger proportion of respondents said their health and wellbeing had got worse than improved since March 2020 and this was more likely to be the case for females than males. Thought should therefore be given to supporting women access services, particularly in deprived areas, where the survey shows community support has weakened to a greater extent than more affluent areas.
- There is evidence that availability and access to health and social care support services plays a large part in people's health and wellbeing. Consideration should be given to how services communicate and engage with the public to improve access as we come out of COVID-19 restrictions.
- The responses to the open questions strongly indicated the pandemic's impact on people's general mental health, those suffering mental illness who were unable to receive face-to-face support, as well as the impact of loneliness – particularly for the elderly.
- Support from the community since March 2020 was evident from the survey responses. This shows the importance of local volunteering and local community groups during this pandemic. However, an important response to note is that over twice as many respondents from the most deprived communities stated that their community had got weaker than average. This should be considered in future planning.
- The public have embraced new methods of consultation or contact with healthcare or social care professionals such as video calling, telephone consultations and updating information via text message and virtual visiting. In future, offering digital methods along with traditional methods would enable people to choose the method that meets their needs, taking into account learning around digital exclusion.
Key findings
Your health and care experience
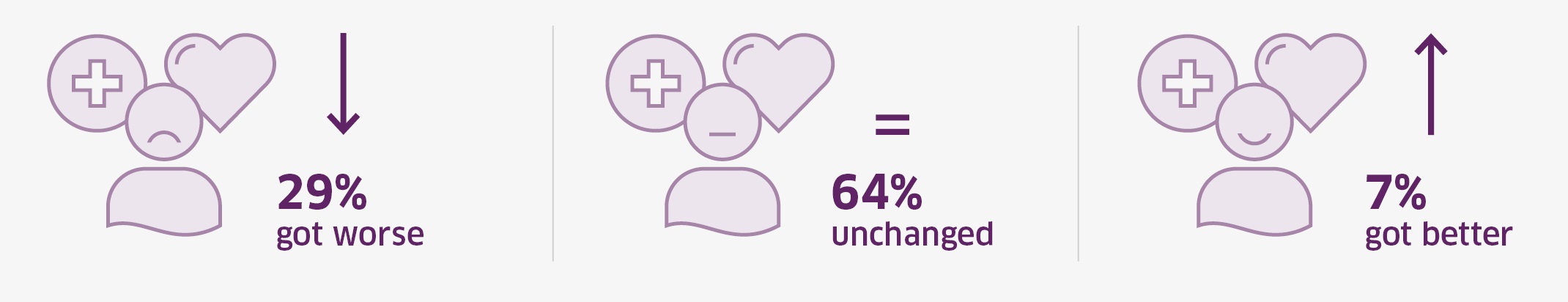
- The majority of Panel members (64%) said their health and wellbeing had remained about the same since the COVID-19 restrictions began in March 2020. On the other hand, 29% of respondents said their health and wellbeing had got worse – which is around 4 times more than the proportion of respondents who felt their health and wellbeing had improved (7%). Females (37%) were more likely to say that their health had got worse than males (20%).
- The survey asked respondents about any changes they have made in relation to their health and wellbeing since March 2020. The vast majority said they had seen no change in relation to taking medicine (74%) and healthy eating (63%). On the other hand, activities that respondents were most likely to be doing more often included exercising (38%), keeping in touch with friends and family (31%) and eating healthily (23%). It is interesting to note that keeping in touch with friends and family (28%) and exercising (26%) were also the activities respondents were most likely to be doing less often.
- Routine appointments opening back up (73%) was the top priority for respondents when asked about their priorities for support from health and social care organisations to improve their wellbeing over the next 6 months. This was followed by better access to GP services (65%) and shorter waiting times to access services (53%).
- Just under two thirds of respondents (65%) had accessed or tried to access health and social care services since the pandemic started in March 2020. The majority of respondents had tried to access their GP (80%). Females were more likely to have accessed or tried to access services (71%) than males (58%).
- Just under half of respondents who had accessed, or tried to access, health and social care services during the pandemic said they had difficulty accessing these services (49%). The most common reason for having trouble was due to longer waiting times to access the service (62%), unable to contact the service (40%) and poor communication (30%).
- One third of survey respondents (33%) had avoided accessing health and social care services and support during the pandemic when normally they would have accessed them. The most common reason for avoiding services was a reluctance to burden or put stress on the NHS (27%), followed by experiencing difficulties in getting an appointment (20%).
- Just under 7 in 10 respondents (69%) had contact with a health care professional and 8% with social care services since the pandemic was declared in March 2020. Respondents were most likely in both instances to have made contact via a telephone consultation.
- Around half of respondents considered their appointment with a health service (50%) or social care service (53%) to be about the same as normal. Those who had contact with a health service were more likely to say their appointment was better than normal (19%) than those who had contact with a social care service (5%).
- The majority of respondents would be willing to see a health or social care professional via online tools such as video consultations (64%) and via telephone consultations (58%) if it meant health services could resume. Over half of respondents (55%) said they would be willing to update information on their condition or wellbeing through an app, text or website if it meant health services could resume. Those in the 65+ age group were less likely to say they would use video or telephone consultations or an app, text or website.
- 30% of respondents had missed routine appointments, with the most common reason being due to appointment cancellations or appointments being on hold due to the pandemic (64%).
- Phoning 111 was the top response for respondents when asked who they would contact if they required medical help for someone quickly and their situation wasn't immediately life threatening (53%). 30% of respondents would contact their GP, 21% would access NHS inform and 15% would contact their pharmacy.
Virtual visiting
- Almost all respondents had not used any form of hospital virtual visiting since the COVID-19 pandemic started in March 2020 (93%). On the other hand, 2% had used this as a patient, 5% had used this as a family member or carer and 1% had used this as a member of staff.
- Few respondents (47) had used virtual visiting but for those that had the vast majority (88%) were satisfied with the experience.
- Over 8 in 10 respondents (82%) said it was very important or important for this option to be available in the future.
Support from your community
- One in five respondents (20%) said that their health and wellbeing has been supported by the community since the COVID-19 pandemic started in March 2020. This support was most likely to be having someone to chat with (65%), receiving help with shopping (49%) or receiving help collecting a prescription (31%). Those in the 65+ age category were more likely to have stated that they received support by the community (30%).
- Just 12% of respondents who had not received support from the community said they would have benefited from support if it were available. When asked about the nature of the support which would have helped them, this was consistent with the most received types of support with 63% saying having someone to chat with would have been useful, 31% would have liked to have received help with shopping and 20% would have benefited from help to collect a prescription.
- Over half of respondents had seen no change in the strength of their community since the COVID-19 pandemic started in March. However, 36% felt their community had strengthened compared to 11% who felt it had weakened. Those respondents from the most deprived communities were more likely to state that their community had weakened (24%).
What matters to you?
The survey included 3 open-ended questions asking respondents to describe their priorities for their own health and wellbeing, for health services and for social care and support services over the next 12 months. The responses were coded into common themes for analysis purposes. The key findings were:
- Priorities for individual health and wellbeing: Being healthy, safe and well was the top priority for respondents (30%). This was followed by access to health services or for services to resume (25%), a COVID-19 vaccine or other COVID-19 concerns (17%) and being able to see family and friends again (17%).
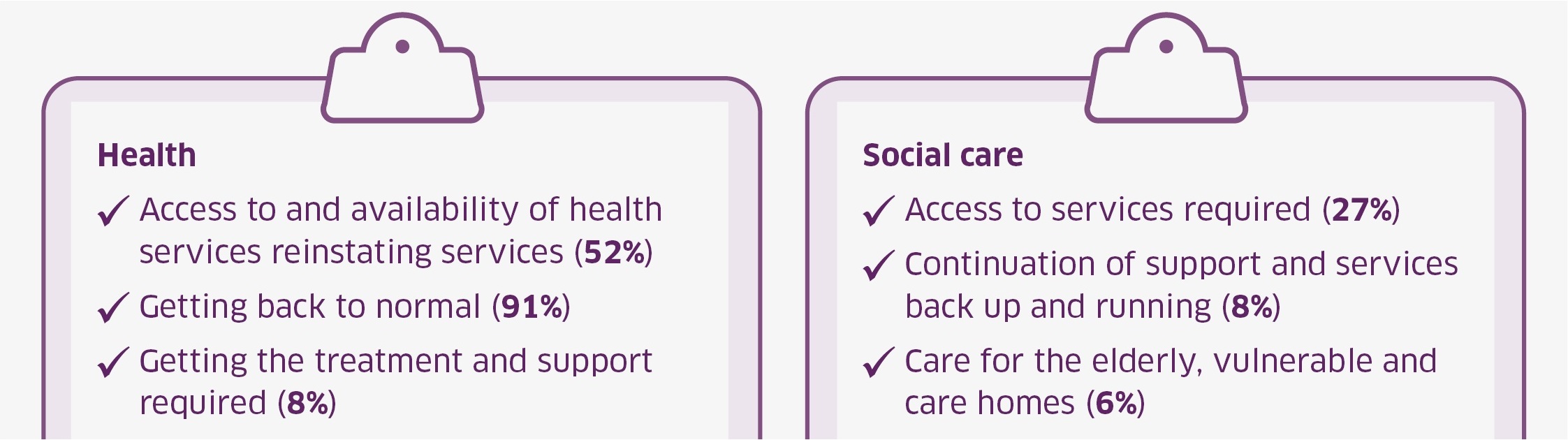
- Priorities for health services: Over half (52%) cited access to, or availability of, health services or for services to be reinstated. This was followed by getting back to normal (9%), getting the treatment or support required (8%), face to face appointments (8%) and timely access or better waiting times (7%).
- Priorities for social care and support services: The top response was access to these services if required (27%), followed by continuation of support or seeing services back up and running (8%) and care for the elderly and vulnerable or those in care homes (6%).
Impact
The panel provided very helpful and timely public feedback on key issues affecting health and wellbeing during the pandemic. This was particularly useful as we were limited in carrying out engagement due to COVID-19 restrictions, and the survey focused specifically on recovery and renewal following COVID-19.
The findings from the Panel survey were an important addition to the body of evidence on the widespread and serious impact of COVID-19 on people's experience of health and social care. They were shared with the Cabinet Secretary for Health and Social Care, Health and Social Care Directors in Scottish Government, and NHS Board Chief Executives, and looked at alongside further public engagement findings, for example the Health, Wellbeing and the COVID-19 Pandemic report by Alliance
Key themes from the findings, such as the need for a person-centred approach to service design and delivery, were used by Scottish Government to develop the mission, objectives, and work programme for the Care and Wellbeing portfolio. For example, this includes recognising that:
- Health and wellbeing is dependent on other factors and services.
- People are aware of what impacts on their wellbeing and want to be involved in co-designing solutions.
- A holistic approach is needed in supporting health and wellbeing, for example recognising the role of unpaid carers or the range of other factors that might influence wellbeing.
The findings from this survey were also selected to be presented at the NHS Scotland national event in June 2021.